by Mitch Hauschildt, MA, ATC, CSCS
The other day I posted a video on social media of me discussing Janda’s Lower Cross Syndrome in a recent seminar. It’s something I discuss a lot in almost all of my seminars because it is so important to understand and it is so prevalent in our culture.
This syndrome was presented by Janda over 30 years ago and is very common in our society because of all of the time that we tend to spend sitting in cars and chairs. Our comfortable lifestyle feeds this dysfunction, which is characterized by shortened and overactive hip flexors and lumbar extensors that are correlated with lengthened and underactive lower abdominals and glutes.
One thing that I mentioned in my video is a list of all of the negative issues that can arise in conjunction with Janda’s Lower Cross syndrome. Because I’m always interested in the “why”, I’m sure many others are as well, so I thought it would be good to take a minute and unpack how lower cross is related to all of these issues. This in not an all encompassing list, but a good start.
Foot Pronation:
- It’s been long established that foot pronation, recurvatum at the knee and anterior pelvic tilt all go together. This is a classic stance for young people who don’t have a lot of tone naturally and struggle to create stability. They rely on their bones and ligaments for structure and not their stabilizers. Most of the time we think of this posture as originating at the foot, which it certainly can. But, it can also go top down. The reality is that I don’t really care where it is originating. If I know that they are all associated, I better address all parts of the problem. So, instead of just throwing them in some orthotics and hoping it fixes things, I prefer to address the lower cross issue at the hips and teach stability at the foot and lower leg at the same time.
Ankle Sprains:
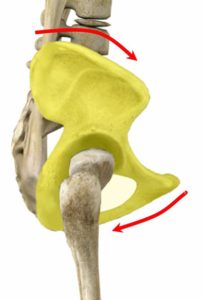
- Research tells us that shortly after an ankle sprain occurs, the gluteus medius has a propensity to turn off. That tells me that through some sort of a neurological connection (that is another discussion all together) the ankle and glute med are tied together. Where lower cross comes into this discussion is that the glutes can’t perform optimally in an anteriorly rotated pelvic position. It’s impossible. So, if I know that the glutes are connected with the ankle, then I can surmise that lower cross syndrome can be a contributor to poor ankle stability and motor control.
Patella Femoral Comprehension Syndrome (PFCS):
- PFCS is everyone’s favorite junk term for that knee pain that isn’t surgical, but physicians don’t quite know what to do with it. The traditional thought is that the pain is caused by a laterally tracking patella that is usually caused by a poor functioning VMO. We now know that PFCS is much more a product of what is going on above and below the knee. If the glutes aren’t working well to control the femur and they allow it to fall inward into valgus and internal rotation, knee pain will ensue. We just established above that the glutes can’t function optimally when someone is stuck in a lower cross pattern. Of course the foot pronation issue that we also discussed previously is part of the problem as well.
 ACL Tears:
ACL Tears:
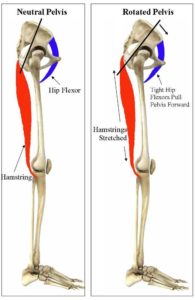
- This is an area that many people don’t consider when looking at Janda’s lower cross syndrome. There are several ways lower cross syndrome exposes athletes to ACL tears. First, just was we discussed with PFCS, if the glutes can’t perform well, femoral control is going to be problematic at best. The most common mechanism for an ACL tear is foot pronation, tibial internal rotation and valgus at the knee. All of these are associated with ACL tears. To make things worse, the hamstring is also intended to unload the ACL in the knee. Because of the anatomical position of the hamstring (starts on the ischial tuberosity and inserts on the tibia), when it shortens, it pulls the tibia back into the knee joint, thus unloading the ACL. In a lower cross pattern, the hamstrings don’t work optimally because they are lengthened all of the time and thus struggle to do what they are designed to do.
 Hamstring Strains:
Hamstring Strains:
- As discussed in the ACL section, with lower cross, the hamstring is constantly in a lengthened position. Sooner or later the hamstring will give way while sprinting with a lower cross pattern.
Hip Flexor Pain:
- It can be argued that the hip flexors are the most dysfunctional muscles in the body. They can be short, long, overactive, underachieve and painful all at the same time depending upon what the body is asking of them. With lower cross, they are shortened and tend to be “on” a lot more than we would like because they are trying to make up for the lower abdominals not doing their job. They essentially become a stabilizer when they are intended to be more of a prime mover. Sooner or later this will become problematic. Another way they become a problem with lower cross is that when a person goes into hip flexion in this postural position, oftentimes the hip flexors get pinched between the pelvis and femur and become painful.
Low Back Pain:
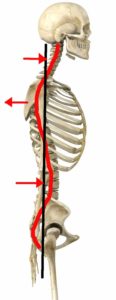
- When the pelvis goes into an anterior pelvic tilt, the lumbar spine has to go into excessive extension. This leads to the spinous processes to jamb into each other, creating pain and all kinds of issues in the low back.
Thoracic Kyphosis:
- Because the spine is always looking to find a center line, when the pelvis rocks anteriorly, the lumbar spine goes into extension and then the thoracic spine has to go into flexion. This kyphotic position can be painful in and of itself, leading to things like compression fractures with some people, but also tends to contribute to a lot of other upper extremity dysfunction that ultimately becomes painful.
Shoulder Dysfunction:
- When the thoracic spine becomes kyphotic, shoulder stability is compromised. Scapulothoracic rhythm becomes abnormal which often leads to shoulder impingement and in a worst case scenario, instability, labral tears and/or rotator cuff issues.
Neck Pain:
- As we follow the dysfunction up the spine, we find that if the thoracic spine goes into flexion, the cervical spine has to go into excessive extension in order to be able to look around and see the world around you. Just as with the lumbar spine, this causes pain from the vertebrae jamming together and eventually can lead to further damage to other surrounding tissues.
I hope this doesn’t read as a death sentence to someone who presents with lower cross syndrome, because there are definitely worse physical ailments to have. But, I also hope that this sheds some light on why it is so important to recognize and address the dysfunction that is Janda’s Lower Cross Syndrome.


Again all great stuff. Could this also cause Achilles Tendon to be under a lot of stress? Causing inflamation and pain when walking or just sitting?
Definitely. I can cause the entire LE posterior side to be on stretch. I think you would tend to see it more when walking than sitting, but I won’t rule either out.