by Mitch Hauschildt, MA, ATC, CSCS
I always get a few interesting faces in the crowd when I make the statement at my courses that plantar fascia pain is rarely coming from the plantar fascia. As much as we would like to think that plantar fascia pain is coming from the foot, because it would be a lot easier to deal with if it was, it rarely is. I 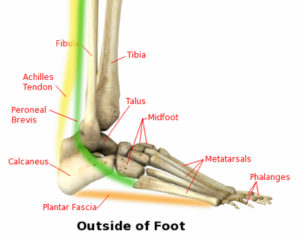 have seen it over and over. I find that it is almost always coming from some biomechanical issue somewhere else in the kinetic chain and the foot is the weak link in the chain. That is why things like massage, cold rollers, calf stretching routines, different shoes, medications, injections and night splints rarely completely solve the issue. Those items usually decrease pain for at least a while, but rarely do they get rid of it all together or for good.
have seen it over and over. I find that it is almost always coming from some biomechanical issue somewhere else in the kinetic chain and the foot is the weak link in the chain. That is why things like massage, cold rollers, calf stretching routines, different shoes, medications, injections and night splints rarely completely solve the issue. Those items usually decrease pain for at least a while, but rarely do they get rid of it all together or for good.
In an effort to understand some typical restrictions that often cause plantar fascia pain, I thought it would be good to discuss some of the areas of the body that typically contribute to foot pain. Hopefully this will provide some understanding in an effort to help you solve this problem for good. Of course, this isn’t an exhaustive list, but a good place to start. I am listing them from the ground up, and not necessarily in any order of importance.
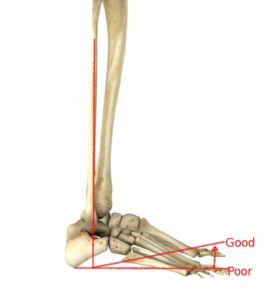
- Big Toe Extension
- This is a classically overlooked restriction. Poor extension will force the foot to compensate in some way. Oftentimes to get around the lack of mobility, the foot will over pronate during push-off, causing excessive strain on the plantar fascia.
- Mid Foot Mobility
- As classically defined by the Joint by Joint approach, the midfoot should be stable. While this is true, I also find that a mid foot that is restricted will cause significant issues with Ankle Dorsiflexion. Naturally when you have a lack of Ankle Dorsiflexion, you will have a tendency for Plantar Fascia Pain. You can learn more about midfoot mobility in another one of my posts here.
- Mid Foot Stability
- Ankle Mobility
- This is the classic culprit that most people go after. While this can be the issue, it is often related to other issues in the kinetic chain. When it is directly related to lack of ankle mobility, we need to make sure we understand the best way to approach it. Most people attempt to improve ankle dorsiflexion by stretching the calf. Unfortunately, most people are restricted in the ankle because of a joint restriction, not a gastroc restriction. Thus, stretching the calf rarely helps. An ankle joint restriction needs to be treated with ankle mobilizations. Check out my blog post here for help in this area.
- Tibial Internal Rotation
- I have documented the need for Tibial Internal Rotation well in the past. Most people that I come in contact with struggle in this area. Poor Tibial Internal Rotation will often lead to excessive pronation and valgus at the lower leg. This can lead to plantar fascia pain over time.
- Proximal Tibiofibular Joint
- Related to poor ankle dorsiflexion, if the fibular head is sitting posterior compared to where it should be (rather common), it will push the distal fibula anteriorly, reducing dorsiflexion.
- Knee Stability
- If someone has poor stability in their knee due to a previous injury, such as a ligament tear that hasn’t healed properly, their body will attempt to rob stability from their ankle to make up for their lack of stability at their knee. This will ultimately lead to poor ankle mobility and plantar fascia pain.
- Hip Mobility
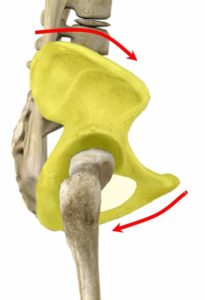
- The hips are supposed to be mobile and in a neutral position. If they are lacking hip mobility, several things can happen. First, they may attempt to steal mobility from somewhere else in the chain, such as the mid foot, which is supposed to be stable. This will create a stability problem which ultimately can lead to foot pain. This has long been observed in the relationship between anterior pelvic rotation and foot pronation that we know can go from the bottom up and top down. The other example that comes to mind that connects pelvic position and the foot is the understanding that there is a direct neurological connection between glute function and ankle dorsiflexion. If the glutes don’t work well, oftentimes the ankle doesn’t dorsiflex well and vice versa. Fixing one is tough without fixing the other.
- Trunk Stability
- If the core and trunk stabilizers aren’t working efficiently, the entire kinetic chain is affected. We can look at this a number of ways. The diaphragm is the neurological driver for the entire lower extremity. If someone doesn’t have trunk stability, they oftentimes steal it from the hips, causing them to be immobile and that leads to all of the things listed above. When someone decelerates without trunk control, the upper body continues to drift, shifting the load to other parts of the body (such as the foot) causing overuse issues. And I can continue…
- Thoracic Spine Mobility
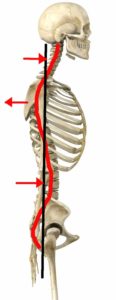
- The Thoracic spine can be considered a linchpin of movement. If the thoracic spine isn’t mobile, it will cause a ripple affect throughout the body. To provide an example of this, if someone has a kyphotic posture, it will cause lumbar extension which will lead to an anterior pelvic tilt and either an ankle dorsiflexion restriction or over pronation.
- Cervical Spine Mobility
- We can take the explanation used above with the Thoracic spine up the chain (spine), which causes all of the same ripple effect as above. A head forward posture is related to kyphosis, lumbar lordosis, anterior pelvic tilt and ultimately foot issues. Further, if the cervical spine is not working well, the brain’s ability to control the body is limited because everything moves through the region of the neck. If we want to improve movement, many times is should start at the cervical spine.
- Shoulder Stability
- The glutes are important for foot pain, as discussed above. The glutes work in conjunction with the opposing scapular stabilizers through the thoracolumbar fascia. If the shoulder complex is not stable, usually the glutes aren’t working well either and it will continue down the chain.
- Grip Strength
- Grip strength is directly related to the rotator cuff. It is a way that the brain protects the shoulder joint by limiting grip when it is hurting. The rotator cuff is important for shoulder stability and if it isn’t working well, we can continue down the chain as demonstrated above.
Overall, there are a number of factors that can lead to or contribute to plantar fascia pain. Some of these are more likely than others, but my point with this post is to encourage those clinicians who are treating plantar fascia pain to look far beyond the foot itself. The goal is to find dysfunction somewhere in the chain and fix it. That is how we find permanent, long term solutions for this common problem.


Leave a Reply