by Mitch Hauschildt, MA, ATC, CSCS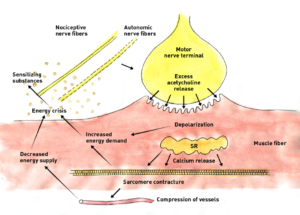
One of the very first questions that I get when I talk about Dry Needling is “how does it work?” Of course, the answer is, it is complicated. And, quite honestly, we don’t always know the exact mechanism as to how this and a lot of our other treatments work. What do know, is that we see them working in our clinics and facilities every day.
Before I jump into this topic, I want to be clear that the information that I’m presenting here is my interpretation of what I think is happening after reading about the topic and seeing and watching it first hand for several years as a clinician. There are lots of smarter people than me that can use larger words than I can to really dial into what is going on when we insert a needle in to tissue, so if you are looking for that, keep looking. However, if you are looking for someone to dial it into what seems to be important to for the clinician to understand and relay to your patient, I just might be your guy.
When I think about dry needling, I think of several different categories of effects that we experience with our needles. Interesting enough, we see many of these same effects with our other various modalities that we utilize in the rehab world (i.e. cupping, IASTM, taping, flossing, massage, etc). What this says to me is that all of the various tools and modalities that we use are all just different handles to open the door to the human body. Our job is to figure out which handle is best for that specific person at that time.
I’m going to categorize the effects of needling into the areas of mechanical, neurological and fluid management. Let’s be very clear when we talk about these 3 areas in the fact that there is spill over between the 3 all of the time. Meaning, the mechanical effects of the needle will stimulate the nervous system and possibly move some fluid. And, the neurological effects of the needle will also likely improve Hyaluronic Acid viscosity in a specific area, improving tissue slide and glide. So, nothing happens in isolation or a vacuum. It is important that we understand that from the beginning.
Mechanical Effect
This is the easiest place to start conceptually in my opinion because I think that most of us can understand that when we place a needle into tissue, it will get distorted in some manner. How far we go with this concept is really up to us.
The first way that we achieve a mechanical effect is by inserting the needle into the skin. By penetrating the skin, connective tissue and muscle, you are straining fibroblasts and stimulating a healing process. It is assumed that by straining these fibroblasts, that the connective tissue will begin to realign to a more advantageous position. 
We can add to that by twisting a needle that is inserted into tissue. It is believed that by twisting the needle, you are wrapping the fascia and connective tissue around the needle, further distorting tissue and further stimulating fibroblasts.
We can further this process by taking a twisted needle that is “bound up” and lifting the needled. This can be effective for decompressing deeper tissue in a targeted area. One example of this is an advanced needling technique where you insert a needling into the transverse ligament and lift it to decompress the median nerve for someone with carpal tunnel syndrome symptoms. This technique can also be used to improve tissue slide in an area of the body where the fascial layers have become densified.
Fluid Management
This is the effect that I personally utilize the least with my needles. It isn’t that it doesn’t work, it is just a technique that I have found works best with acute swelling due to a fresh injury and in my position at the university, I just don’t see a ton of acute injuries. Many of my coworkers love needling for swelling and swear by it. Think acute ankle sprain or larger contusion for this application.
I personally haven’t seen much convincing evidence as to the exact mechanism for this application, but the technique involves using a lot of very short needles that simply pierce the skin and penetrate the loose connective tissue beneath the skin’s surface (some would call this the interstitium). This space plays an important role in moving fluid from one area of the body to another. By placing needles into the loose connective tissue, we are essentially sending a signal to the brain to start moving fluid out of this area and normalize the fluid content within the local tissue.
Neurological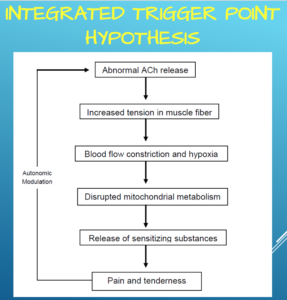
This is by far the most important and most exciting effect of dry needling. While I do believe in the mechanical effects of needling, the reality is that anytime we are touching the skin, we are treating the nervous system. As Dr. Eric Cobb of Z Health always says, “We are always treating neurology, many times by mistake.”
My stock answer when people ask me about dry needling is that I want them to think of it as a “neurological reset.” When we place needles into local tissue, we are increasing the conversation between that area of the body and the brain, making it more aware of what is going on and the brain will normalize tissue. This is very similar to the concept of reflexive activation that Robert Schleipp has described.
He states that when you mechanically stimulate local tissue, it sends a signal to the brain which then changes cytokines and the pH balance, which results in a palpable tissue response. The beautiful thing about this model is that we don’t necessarily have to figure out I the tissue needs to be up or down regulated. Our job is to stimulate the local tissue and let the brain figure the rest out, because it is smarter than we are.
We see this with needling in local trigger points. We can change tone simply with a needle inserted into the painful and hypertonic tissue. We know that trigger points are primarily a nervous system response because they don’t exist in cadavers. And, we also know that the local tissue around a trigger point tends to be more acidic in nature (change in pH). When we insert a needle into a trigger point, we are talking to the brain, which then changes the pH balance and we get a palpable tissue response in the local tissue.
But, there is a lot more to consider with regards to the nervous system and needling. One area that a lot of research is focusing on is peripheral and central centralization. This is a HUGE topic that can consume a series of blog posts just by itself, so we are going to keep this part of the conversation very high level and simple.
We are going to define peripheral sensitization as the lowering of the threshold for a nervous system response that leads to hyperalgesia (extra sensitive response). For this response, think about a very sensitive and painful area that responds to a low level of stimulus. I also consider peripheral sensitization as more of a local, bottoms up pain response that originates in the disrupted tissue.
Research is demonstrating that dry needling can have a pretty robust effect on peripheral sensitization. It is rather complicated and quite honestly, above my head, but we are understanding that by inserting a needle into the local tissue, we are changing the feedback loop and actually alters the end neurotransmitter response as it interacts with the end plate, ultimately changing local tone and nociception (pain). This local response is what most of us who needle start with as an attempt to get people moving and feeling better quickly.
What I think is actually more interesting is the impact that we are seeing on central sensitization with needles. Central sensitization is more of a top down mechanism that causes pain. This is when our brain gets caught in a cycle of chronic pain that may or may not be caused by a specific noxious stimulus. It can be a bit scary as a clinician because if pain evolves to a point where it is centrally driven, it can be very hard to deal with.
There is limited, but interesting data that is suggesting that dry needling can down regulate central sensitization. This can be done by needling an opposing limb in a similar painful area (myotome) or by needling a part of the body that is a good distance from the chief complaint (i.e. needling a calf for shoulder pain). If we can truly dial into where and when to needle different parts of the body to impact central stabilization, we truly will be able to solve a lot of chronic pain issues.
Parasympathetic Response
Another indication of the nervous system response to needling is the way that it impacts the sympathetic and parasympathetic nervous system. If I am trying to reduce pain, I want to stimulate a parasympathetic response. This down regulates nervous system tone and makes for a more peaceful, happy individual.
What we see with a number of patients after a dry needling session is that they become very relaxed and sleepy, indicating a parasympathetic response. This should be encouraged and celebrated. Let them relax and take a nap. Encourage them to not perform stimulating activities after needling. Activation of this part of the nervous system is great for reducing pain and improving overall movement health.
Conclusion
There are a number of ways that Dry Needling can impact the body and help our patients. It can also be intimidating to many of them, so time should be spent prior to needling someone for the first time to educate them and make them comfortable. I have laid out several proposed mechanisms of dry needling and I’m sure we could have a really great discussion if we wanted to expand on these principles and I’m sure 5 years from now, we will have greater understanding of the hows and whys. Until then, we can work with these principles and explore new concepts and parameters in an effort to make our patients better and learn whats nest for this exciting tool.


Leave a Reply