by Mitch Hauschildt, MA, ATC, CSCS
I’ve said recently that the evaluation process is by far the most important part of your training or rehab program. If you don’t know your patients or clients, you can’t give them the proper interventions. What I didn’t address in that post is, what does a proper screen really look like?
Screen vs Assessment
First, it is important that we understand the difference between a screen and an assessment. A screen is basically examining a patient or client to see if they are suitable for a specific movement or task. The goal here is to identify gross abnormalities that may limit their performance, cause pain, or ultimately lead to an injury. Screens are to be done in the absence of pain. A screen is not specific enough to diagnosis an injury or problem.
On the other hand, an assessment should be performed with painful patients. An assessment is much more detailed in nature and involves our clinical decision making skills (for those of us who are clinicians). An assessment should ultimately lead us towards a diagnosis and origination of painful or dysfunctional areas of the body.
For this post, we are focusing on a screen and the various components.
For a number of years, I have been a big proponent of the Functional Movement Screen (FMS) as an important part of the screening process. I have been performing FMS’ since 2001 on athletes of all ages and levels of activity and it has proven to be a valuable piece of my understanding of a patient or athlete.
While many people have described me as an “FMS guy” over the years, I have also been critical of the FMS over the years and it’s limitations. I think it is a very valuable tool for getting a quick snapshot of an athlete in a few minutes, I also would like to see something different done with the rotary stability and shoulder mobility tests to help those who are performing the screen better understand the proper interventions. I have personally attempted to create a better system in these areas, but unfortunately, I’m not bright enough to find a better way yet.
There are a numbe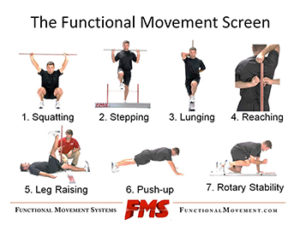 r of advantages of using FMS such as:
r of advantages of using FMS such as:
- It is supported by research studies (sometimes mixed reviews on it, but the majority is positive).
- It has a systematic scoring system that results in specific numbers based on performance.
- It provides a common language for those who know how to use it that can be easily communicated among multiple people working with the same patients.
- It has some planned redundancy built into it to give you a good road map for what is limiting an athlete’s ability to move well.
- It gives a really good snap shot of an athlete that you don’t know or haven’t seen in a while in less than 10 minutes.
The disadvantages of the FMS system as I see them are:
- The scoring system leaves a ton of space in the “2” category. Meaning that there is a huge spectrum of compensations that allow you to get a 2. This can make it difficult for some novice users to make good use of the screen.
- It only assesses people in a slow, controlled and unweighted manner (which is honestly their goal, but doesn’t always match up with an athlete’s needs and is why they recently introduced the Functional Conditioning Screen).
- You need equipment to perform it which at times makes it cumbersome to take on site.
- It can feel time consuming for many people to perform the FMS. In my setting, I see my athletes daily for several years, so I can almost always nail their FMS score just because I know their training habits, body style, and dysfunctions well. Thus, sometimes screening seems a bit repetitive for us in our setting.
Based on this, I use the FMS as a major part of our injury screen process, but I augment it with several other tools in order to get a better view of what is really going on with my athletes. We use these 4 components to fully screen our athletes in the college setting:
- Lumbopelvic Evaluation: We perform this supine and look for any kind of a rotation, upslip, and/or leg length discrepancy.
- Foot Mechanical Evaluation: We look at mobility, stability and function in both weight bearing and non-weight bearing to see how their foot mechanics affect the rest of the kinetic chain.
- Functional Movement Screen: Assesses movement in a controlled environment.
- Hop, Stop and Leap Test: Looks at single leg power and deceleration and symmetry in each.
The only other area that I would like to integrate into my screen at some point might be something with a load and/or under fatigue. I would like to have an indication as to their quality of movement under these conditions as well for the perfect screen, but at the end of the day, that would increase the time and complexity of a screen so I have to rely on our strength and conditioning staff for some of that information from time to time.
I’m not as concerned that you use my system as I am that you actually have a system
I have said this a lot over the past few years. What I find isn’t that most people are using the wrong system, it’s that they just don’t have a system at all. There is no process in place for really evaluating how someone moves and then what to do about it.
If you decide that you are going to establish your own screening process, here are some important points that should be included in the process:
- Biomechanical Screen: Every body is different and it is important that we consider these variances when looking at movement quality and injury risk.
- Movement in an unloaded, controlled environment: Including looking at the following elements:
- Squat
- Lunge
- Press
- Pull
- Rotation
- Plank
- Deceleration: Many people get injured when attempting to slow down under a load.
- Power: A powerful person is less likely to be injured.
- Symmetry: Asymmetries are the second highest predictor of injuries behind previous injury.
Remember that all movement can be a screen when you standardize the task and analyze it in all 3 planes of movement. Understand the demands of your patient’s activities and life in general and create a movement screen that matches what they do. Then, of course, set high expectations of them and help them reach those expectations.


Leave a Reply