by Mitch Hauschildt, MA, ATC, CSCS
Recently, I came across an article from the Journal of Orthopaedic and Sports Physical Therapy discussing ACL rehab entitled, “Neuroplasticity Following Anterior Cruciate Ligament Injury: A Framework for Visual-Motor Training Approaches in Rehabilitation.” Anytime I see something about ACL injuries and rehab involving the brain, I perk up and take notice.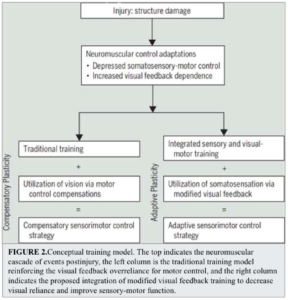
The article is well written and interests me because they are tapping into an area of orthopedic rehab that is really intriguing and has been a big focus for me in the past year or two. The concept of neuroplasticity and somatosensory retraining as part of sports medicine rehab makes a ton of sense and has been largely underappreciated for many years.
If you haven’t yet read (please follow the link above and read it), the basic premise is that after an ACL injury, an injured patient will have decreased feedback from from their leg to the brain, thus they tend to rely more heavily on their visual system to understand where they are in space than they did prior to their injury.
The authors present a very strong argument supporting their claim and they back it up with research. They state that “the loss of primary afferent information combined with the pain and inflammatory response contribute to fundamentally alter somatosensory feedback.” They go on to explain that “these deficits in neural function are not rectified with ACL reconstruction and may become even more pronounced and/or present bilaterally.”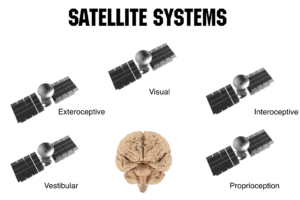
Basically what they are saying is that the GPS system that our brain relies on to create movement and keep us safe is altered after an ACL injury. We talk about the human GPS system in a lot of Rocktape FMT education courses. There is a big parallel to how the brain relies on visual, vestibular, prioprioceptive, exteroceptive and interoceptive feedback to know where it is in space and to ultimately help us move efficiently. When part of the system breaks down, the brain’s perception of the body becomes altered and we don’t move as efficiently as we could. Mosely and Butler would refer to this a smudge on the brain. We have discussed smudges in earlier posts, so feel free look at the archives for more information.
The authors of this article argue that just because you reconstruct the ACL does not mean that the GPS signal will be regained. Reconstructing the ACL simply makes a mechanical improvement and may help with physical instability, but it doesn’t rectify the issues that the brain has developed during the injury process. That will only happen with sensorimotor retraining.
When the smudge occurs, the brain begins to rely more heavily on the visual system for input than prior to the injury, according to the authors. Because of this, they argue that in order to adequately improve the somatosensory system, you need to intentionally modify the visual input into the brain to essentially force the brain to rely on the mechanoreceptors in the body to do what they are designed to do, reverting to a more native movement pattern.
I do like their novel approach to therapy with the use of glasses and vision disruption and it makes sense in a lot of regards. However, I don’t think altering vision is the only way to achieve the desired outcome of a more natural communication between the brain and an injured part of the body.
Anything that stimulates mechanoreceptors in the skin and fascia will assist in this process. That may be manual massage, IASTM, tape or other intervention. This is using exteroception and the direct connection between the skin and the brain to our advantage. We have seen great success with some of our longer term rehab programming with graphesthesia and tactile acuity training in recent months. These techniques help the brain reconnect directly with an area of the body that may have an altered perception of its environment.
As I read this article, it also reminds me why it is important to use feed forward mechanisms wisely in our exercise progressions. While there is something to be said about actively asking our clients to “turn something on” in an effort to regain control over certain parts of the body, if that cuing is always used and becomes dominant, the brain may have trouble establishing it’s own internal cuing, timing and sequencing. I agree with the authors when they state, “Rehabilitation guidelines that focus on explicit feedback (e.g., contract quadriceps or keep knees over your toes) might be further promoting the top-down cortical and visual feedback control of the movement, as opposed to facilitating a return to a more autonomic somatosensory feedback control and visual feedback on the environment.”
My final thought that comes to mind on this topic is the importance of combining our modalities to improve cortical mapping. Using things like vibration (i.e. platforms, manual vibration of tissue, oscillating bands, etc), Reactive Neuromuscular Training (RNT), unstable loads (i.e. sand or water filled implements), with our corrective exercise can go a long ways in retraining the body’s natural movement patterns by providing variety and stimulation from the bottom up instead of the top down. As an side note, we should also utilize these same techniques with our “healthy” athletes to improve their input to the brain to reduce injuries before they happen.
Overall the big take home from this article is that the brain is so much more in control of our movements than most of us have previously appreciated and it can easily become altered through an injury. If we don’t take the correct approach with our therapy, we will never reduce the risk of future injury.


Would it be possible to apply this technique with full knee replacement?
Absolutely!